Understanding the Patient’s Needs in Migraine Management: The Right Plan for the Right Patient
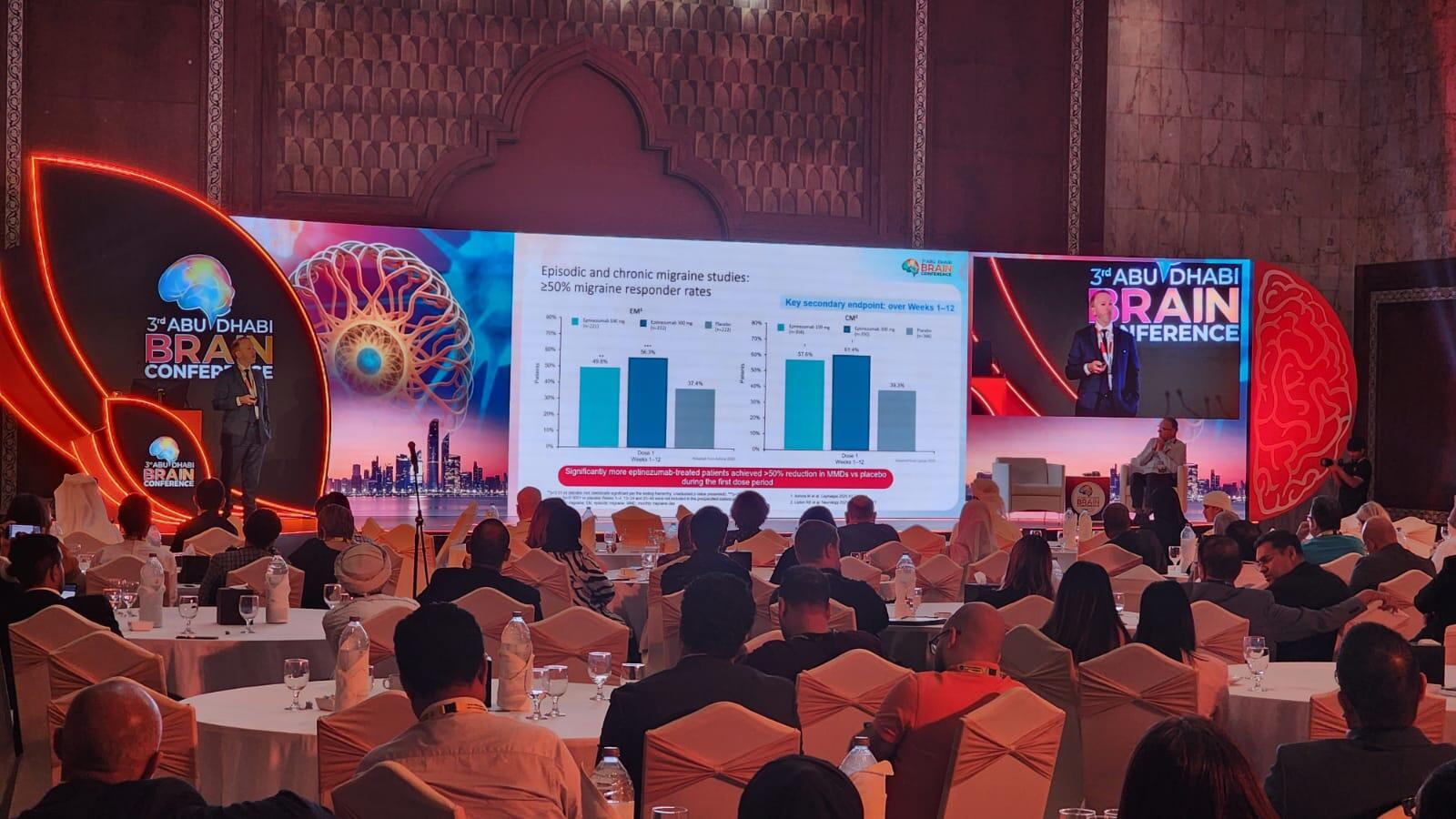
During The 3rd Abu Dhai Brain Conference held in Abu Dhabi, UAE (15 September 2023), the symposium titled " Understanding the Patient’s Needs in Migraine Management: the Right Plan for the Right Patient" Professor Peter McAllister, MD, FAAN (Co-founder and Medical Director; New England Institute for Neurology and Headache, Stamford CT (USA); and Clinical Associate Professor, Yale University School of Medicine) delved into various key aspects related to migraine. From epidemiology to treatment through risk factors and diagnosis, Professor Peter McAllister covered the migraine field in a clear way that is suitable for both neurologists and non-neurologist physicians.
Mapping the Migraine Phenomenon: A Journey Through Global Impact and Prevalence
In the intricate tapestry of global health, migraines unfurl as an enigmatic force, intertwining with the daily lives of approximately 12% of the world's population, a staggering conclave of over a billion individuals predominantly comprising adult females in their zenith of productivity.1,2 Migraine manifests in two distinct patterns: episodic migraines, witnessed in 18% of women and 6% of men, sporadically punctuate their lives with fewer than 15 headache days per month, while chronic migraines cast a longer shadow, ensnaring 1.3% of women and 0.5% of men in a relentless cycle of 15 or more headache days each month.3 Alarmingly, a substantial portion of this populace, about 60%, remains undiagnosed, navigating the complex corridors of this disabling neurological disease without professional guidance. Recent data further amplify the gravity of the issue, positioning migraines as the foremost cause of neurological disability globally and elevating it to the second leading cause of years lived with disability, thus underscoring the urgent need for comprehensive strategies to understand and manage this pervasive health challenge more effectively.4,5
Step 1: Confirming a Migraine Diagnosis: Differentiating from Other Serious Conditions
Initiating an effective migraine management plan begins with an unequivocal diagnosis. It is essential to meticulously ascertain that the recurring headaches are indeed migraines, steering clear of potential misdiagnoses with conditions that manifest similar symptoms, such as a stroke or hemorrhage. Additionally, a keen diagnostic eye should remain vigilant for arteritis, cerebral venous thrombosis, and reversible cerebral vasoconstriction syndrome, which can easily masquerade as migraines. Furthermore, NDPH, meningitis, and fluctuations in CSF pressure headaches be it low or high, should be prudently ruled out. Finally, a comprehensive evaluation would also consider rare but significant conditions like CADASIL and MELAS, ensuring an accurate diagnosis that paves the way for a targeted and effective migraine management strategy. The typical migraine is manifested with moderate to severe intensity, often unilateral, with a throbbing sensation. Sufferers may experience heightened sensitivity to light and sound, accompanied by nausea or vomiting. These symptoms can exacerbate with physical exertion and may present with or without an aura, occurring in either episodic or chronic patterns.
Migraine Vulnerabilities: Recognizing Risk Factors and Identifying Triggers
Migraine occurrence is often closely linked with a variety of risk factors and triggers. Women are more prone to experiencing migraines, especially with increased BMI and during menses. Psychological factors such as anxiety, depression, and stress, as well as childhood trauma, also significantly contribute to migraine occurrences. Environmental factors like low barometric pressure and lifestyle choices such as physical inactivity can be potent triggers. Moreover, a person's genetic makeup can predispose them to more frequent migraine episodes, underlining the complex network of associations involved in migraine susceptibility.
Migraine Management: Multifaceted Approaches to Treatment
Migraine treatment is a nuanced process that necessitates a personalized approach, carefully designed to mitigate the multifaceted triggers and risk factors identified in each individual. It often combines pharmacological interventions, which may involve preventive medications or acute pain relief, with lifestyle modifications encompassing a balanced diet, regular physical activity, and stress management techniques. For females, managing migraines might extend to tackling hormone fluctuations during menses. Furthermore, cognitive-behavioral therapy can be a powerful tool in addressing underlying issues such as anxiety, depression, or childhood trauma that may be exacerbating migraine occurrences. Importantly, patients are encouraged to maintain a headache diary to identify and avoid potential environmental and dietary triggers, fostering a proactive role in their treatment journey.6
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.