When an extensive biomarker study characterizing diverse aspects of brain function unexpectedly failed to reliably discriminate between the three major psychoses identified by the DSM based on phenomenology — that is, schizophrenia (SCZ), schizoaffective disorder and bipolar disorder with psychosis (BPDP) — the biomarkers were subjected to multivariate analyses. These analyses revealed three biotypes with distinct clinical characteristics distributed across all three DSM diagnoses. At CINP 2018, Carol Tamminga, Lou and Ellen McGinley Distinguished Chair and the McKenzie Chair in Psychiatry, UT Southwestern Medical School, Dallas, TX, explained that the biotypes appear to reflect different underlying pathogenetic mechanisms for psychosis, and hypothesized that identification of these mechanisms will enable personalized therapy of psychosis early in its development to ensure recovery and prevent disease progression.
Professor Tamminga is the spokesperson for the Bipolar Schizophrenia Network of Intermediate Phenotypes (BSNIP) group, a five-center NIH-funded consortium led by five principal investigators in the United States. Together the centers provide a broad range of phenotyping expertise and were tasked with developing a biomarker model for the three major psychosis diagnoses identified by the DSM based on phenomenology — SCZ, schizoaffective disorder, and BPDP.
The BSNIP project
An unexpectedly high overlap in biomarkers were found between schizophrenia, schizoaffective disorder, and bipolar disorder with psychosis
The BSNIP consortium carried out dense phenotying for 933 probands with SCZ, schizoaffective disorder or BPDP, 1043 of their first-degree relatives, and 459 healthy controls. The biomarkers included:
- several measures of cognition
- several measures of eye movement
- electroencephalography (EEG)
- structural magnetic resonance imaging (MRI)
- resting functional MRI
- diffusion tensor imaging
- genetic analyses
- plasma immune measures
- Other data collected included:
- Structured Clinical Interviews for DSM-IV, Positive and Negative Symptom Scale, Montgomery Åsberg Depression Rating Scale, and Young Mania Rating Scale for all probands
- Structured Interviews for DSM-IV Personality for DSM-IV relatives and healthy controls
- Birchwood Psychosocial Function assessments
- personal and family histories
-
The biomarkers showed an unexpectedly high overlap between SCZ, schizoaffective disorder and BPDP, and the overlap was also seen for the phenomenology-based clinical characteristics.
Identification of three new biotypes distributed across all three DSM diagnoses1
The failure to discriminate between schizophrenia, schizoaffective disorder and bipolar disorder with psychosis led to further analyses of the pooled data, which revealed three distinct biotypes
The failure to discriminate between SCZ, schizoaffective disorder and BPDP led to multivariate analyses of the pooled data for the probands, which revealed three distinct biotypes:
- biotype 1 — the least functional biotype characterized by low cognitive control, low sensorimotor activity, high grey matter loss, highest number of relatives with psychosis, and high polygene score
- biotype 2 characterized by low cognitive control (but not as low as that for biotype 1), high sensorimotor reactivity, some grey matter loss and relatives with severe psychosis
- biotype 3 characterized by low sensorimotor activity (but not as low as that for biotype 1), almost normal cognitive control, and normal percentage of relatives with psychosis.
These biotypes were distributed across all three DSM diagnoses and relatives of the probands had the same pattern of biotype as the probands.
Biotypes were distributed across all three DSM diagnoses and relatives of the probands had the same pattern of biotype as the probands
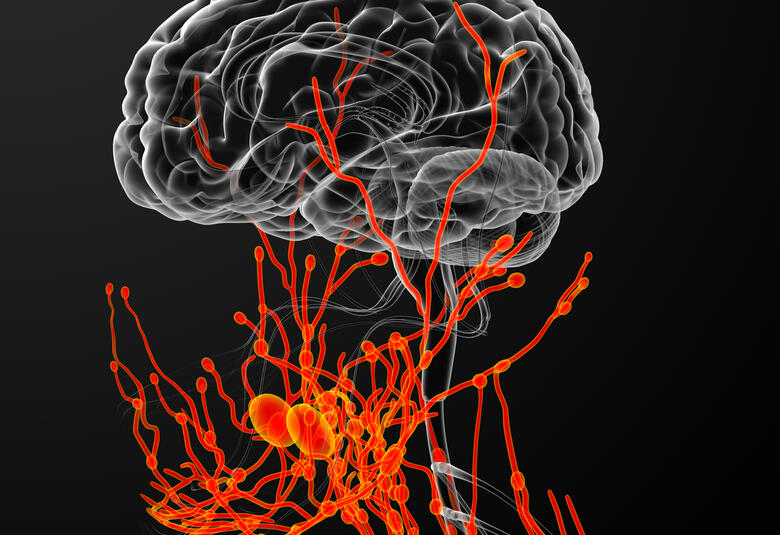
Brain connectivity patterns and Voxel-based morphometry (VBM) analysis differ for biotypes 1, 2 and 3
Further investigations revealed that although brain connectivity patterns look similar to healthy controls for probands when classified as SCZ, schizoaffective disorder and BPDP, they reveal low, high and normal connectivity, respectively, when the probands are classified as biotypes 1, 2 and 3.
VBM analysis by biotype also reveal differences for biotypes 1,2 and 3. Abnormalities are revealed throughout the cortical mantle for biotype 1 probands, but are mainly restricted to the limbic system for biotype 3.
Is psychosis an end manifestation of many different as yet unidentified pathogenetic mechanisms?
Professor Tamminga hypothesized that biotypes 1, 2 and 3 probably reflect different underlying mechanisms resulting in psychosis, and suggested that future research will demonstrate that psychosis is an end manifestation of many different as yet unidentified pathogenetic mechanisms — just as congestive heart failure is the end manifestation of a variety of cardiac, pulmonary and renal diseases.
The results of ongoing and future research hopefully will identify and enable personalized therapy and therapeutic targeting of psychosis early in its development to ensure recovery and prevent its progression
The results of ongoing and future research to identify subtypes of the biotypes resulting from different mechanisms are ongoing, she said. The hope is that such identification will enable personalized therapy and therapeutic targeting of psychosis early in its development to ensure recovery and prevent its progression.